Death By Asphyxiation
The Greek used the term asphyxia when referring to a stopping of the heart rate or pulse. When the body doesn’t get enough oxygen, its organs cannot function, either by inadequate delivery of the oxygen, or poor uptake or utilization of the oxygen by the body’s tissues and organs. This is sometimes accompanied by carbon dioxide retention.
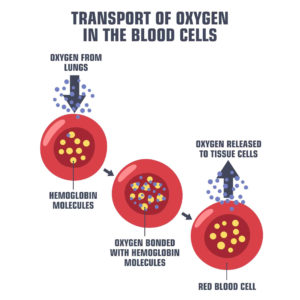
First, normal breathing is impaired, which can lead to unconsciousness or even death. Breathing is also known as ventilation. When a person breathes, they take oxygen into their body via the lungs, which is then processed and spread to the organs and tissues of the body via the bloodstream. This is termed pulmonary gas exchange and gas transport. Then the cells utilize this oxygen to produce energy. Anoxia is the term for a lack of oxygen. How long a person is without oxygen determines whether or not they will have irreversible brain damage. Even a few minutes of complete anoxia can be critical. The brain is the most oxygen sensitive organ.
Death by asphyxiation can be either accidental, suicidal, or homicidal; with three different categories which are strangulation, chemical asphyxia, and suffocation.
Symptoms of asphyxia are shortness of breath, difficulty breathing, a slow heart rate, hoarseness, sore throat, confusion, loss of consciousness, nosebleeds, vision changes, hearing loss, blue lips, and/or bluish colored skin.
There can be many causes of asphyxiation. Diseases such as asthma, lung cancer, chronic obstructive pulmonary disease, emphysema, bronchitis, and pneumonia are all lung diseases that can make breathing very difficult, requiring supplemental oxygen. All of these can ultimately lead to death if the lungs are permanently damaged.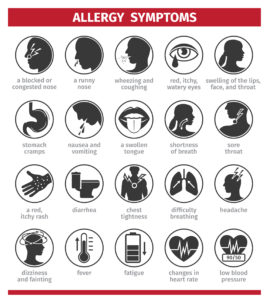
Other methods of asphyxia are things such as foreign objects stuck in the airway or trachea, a severe allergic reaction causing airway constriction, drowning by inhaling water, incorrect body positioning, seizures, drug overdose, or even accidental carbon monoxide poisoning. Carbon monoxide mixes with the red blood cells in the body that are carrying oxygen to the tissues and organs, making the blood incapable of carrying the required oxygen, thus suffocating the cells, organs, and tissues. Strangulation is one obvious way to stop air entering the lungs and blocking blood flow to the brain. This can occur when a hand, ligature, or other object is used to squeeze someone’s throat. There is an act called “autoerotic or erotic asphyxiation” when a person limits their or their partner’s oxygen supply in order to enhance sexual gratification.
Today we will be focusing on chemical asphyxiation. Carbon monoxide poisoning is just one example. Chemical asphyxiation occurs when a substance is inhaled into the lungs and then interfere with the body’s ability to utilize oxygen for survival by either dilution of the oxygen, displacing the oxygen, causing cancer, explosion, penetrating the skin, catching fire, causing birth defects, or damaging the organs directly. Asphyxiant gases derive the body of oxygen and are categorized into simple and chemical asphyxiants. Simple asphyxiants displace the oxygen from the air. Chemical asphyxiants react within the body to interrupt the delivery or utilization of oxygen.
 The most common chemical asphyxiation substances are carbon monoxide, butane, nitrous oxide, carbon dioxide, cyanide, hydrogen sulfide, argon, acetylene, ethane, hydrogen, helium, liquified petroleum gas, natural gas, neon nitrogen, propane, ammonia, formaldehyde, and methane. These types of chemicals can have serious and immediate effects, including unconsciousness and death. There is usually no warning. A few have an odor, but others are odorless. The workplace is the most likely place to encounter these chemicals in confined spaces such as reactors, vessels, tanks, boilers, railcars, trenches, and manholes. Thus, reading the substance’s safety data sheet (SDS) is imperative when working with chemicals.
The most common chemical asphyxiation substances are carbon monoxide, butane, nitrous oxide, carbon dioxide, cyanide, hydrogen sulfide, argon, acetylene, ethane, hydrogen, helium, liquified petroleum gas, natural gas, neon nitrogen, propane, ammonia, formaldehyde, and methane. These types of chemicals can have serious and immediate effects, including unconsciousness and death. There is usually no warning. A few have an odor, but others are odorless. The workplace is the most likely place to encounter these chemicals in confined spaces such as reactors, vessels, tanks, boilers, railcars, trenches, and manholes. Thus, reading the substance’s safety data sheet (SDS) is imperative when working with chemicals.
Of the chemicals listed above, the most insidious are carbon monoxide and cyanide, because they are lethal byproducts of combustion and, with concomitant exposure, increase short term mortality rates by 30-50%. Both of these substances are odorless and colorless causing triage of these patients to be very difficult. It is critical for EMS responders to assess the entire situation in order to effectively treat these patients. People are at increased asphyxiation risk during cold weather because of indoor grill use, gas-powered generators, industrial accidents, natural disasters, suicide/murder attempts, and exposure to combustible materials such as wooden floors, PVC pipes, furniture, paper, plastic, textiles, and other synthetic materials. EMS workers can assess and test for carbon monoxide in the ambient air, but there is no test for cyanide. Sadly, when a person has inhaled these chemicals, pulse oximeters that measure the blood oxygen levels can still show a “normal” reading and thus be misleading, providing false reassurance, leading to a missed diagnosis.
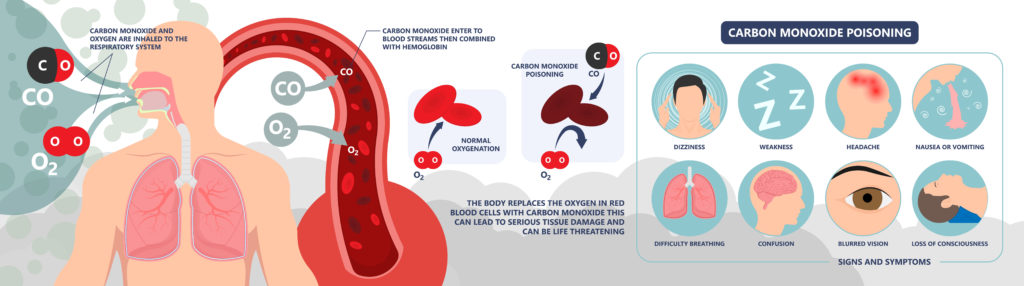
Treatment includes rapid removal of the patient away from the asphyxiant, and supportive oxygen therapy which reverses the lack of oxygen or hypoxia, and also accelerates the elimination of the asphyxiant. This is why hyperbolic oxygen therapy is often used, especially to treat carbon monoxide poisoning.
Homicide due to asphyxia is relatively uncommon, surprisingly. The most common form of asphyxia homicide is ligature strangulation. Other forms of asphyxia death are manual strangulation, suffocation, choking, hanging, and drowning.
We have experts in both strangulation and toxicology that can assist you on your next asphyxiation death case. Contact us today!
Bibliography
Brown, L. M. (2020, Sept 28). What to know about asphyxiation. Retrieved from Medical News Today: https://www.medicalnewstoday.com/articles/asphyxiation
Chemscape. (2022). Asphyxiation Hazards in the Workplace. Retrieved from chemscape: https://www.chemscape.com/resources/chemical-management/health-hazards/asphyxiation
DiMaio, V. J. (2000, Mar). Homicidal asphyxia. American Journal of Forensic Medical Pathology, 21(1), 1-4. doi:https://doi.org/10.1097/00000433-200003000-00001
Graham, M. A. (Updated 2016, Jan 24). Pahtology of Asphyxial Death. Retrieved from Medscape: https://emedicine.medscape.com/article/1988699-overview#a5
Mississippi Encyclopedia Staff. (2018, April 13). Amite County. Mississippi Encyclopedia. Retrieved from https://mississippiencyclopedia.org/entries/amite-county/
Perera, T. B., & Gold, A. (Updated 2021). EMS Asphyxiation and other Gas and Fire Hazards. In StatPearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK519487/
Pierce-Smith, D., Turley, R., & Hurd, R. (2022). Hazardous Substances Demand Your Respect. Retrieved from University of Rochester Medical Center: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=1&contentid=1810
Tan, K.-H., & Wang, T.-L. (2005, Sept 5). Asphyxiants: Simple and Chemical. Retrieved from Disaster.org: http://www.disaster.org.tw/ENGLISH/ann-med/Vol4suppl1/6.pdf
TASA. (2022). Forensic Analysis of Injury and Death by Asphyxiation. Retrieved from tasanet.com.
Don’t miss our newsletter! Topics covered are:
Assault / Trauma
DUI / General Medical
Child & Elder Abuse / Neglect
Mental Health / Toxicology
Sign up here.